Vasectomy surgical Procedure
What is Vasectomy
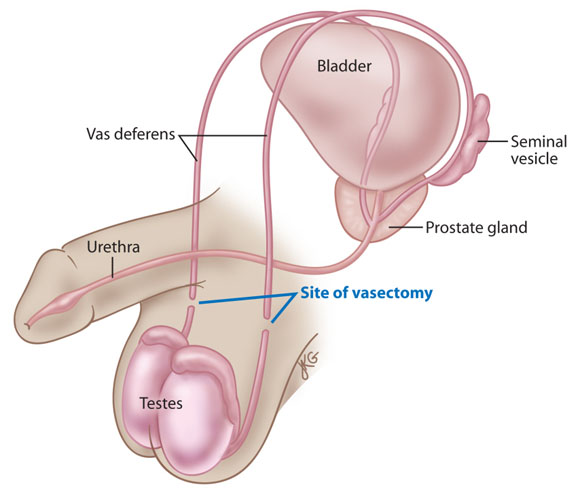
Vasectomy is a surgical OPERATION to sever (cut) the VAS DEFERENS, the narrow tubes that carry SPERM from a man’s TESTICLES to the ejaculatory ducts where the sperm mixes with seminal fluid in preparation for EJACULATION (ejection from the PENIS during ORGASM). One vas deferens extends from each testicle, running very close beneath the surface of the SKIN of the SCROTUM.
Vasectomy Surgical Procedure
There are two methods for performing vasectomy, both of which are outpatient procedures usually done in the doctor’s office. Each begins with the doctor injecting local ANESTHESIA into the scrotum to numb the area. For conventional vasectomy the doctor then makes two small incisions, one on each side of the scrotum, or a single incision at the base of the scrotum. Each vas deferens is accessible through the incision. The doctor cuts each vas deferens, removes a small segment to separate the ends, and sutures (stitches) the ends closed. The doctor then places several small, dissolving sutures to close the incisions in the scrotum.
For the nonsurgical or no scalpel vasectomy, the doctor locates and clamps the vas deferens through the skin of the scrotum using a special instrument called a ringed extracutaneous vas clamp. The clamp closes in a small circle; each tip is sharp. When closed the clamp makes a tiny puncture in the scrotum and pulls the vas deferens through the surface. The doctor cuts the exposed vas deferens, ties or cauterizes the ends, and tucks the sealed ends back inside the scrotum. The puncture heals without sutures. The doctor repeats the procedure on the other side.
Vasectomy procedure Risks and Complications
Some swelling and discomfort is normal during the first 24 to 48 hours after the vasectomy. Ice to the scrotum and one of the NONSTEROIDAL ANTIINFLAMMATORY DRUGS (NSAIDS) such as ibuprofen help relieve INFLAMMATION and PAIN. Wearing tightfitting briefs or an athletic supporter for a few days gives additional support to the scrotum to minimize discomfort. Excessive bleeding and INFECTION are uncommon though can occur, as with any surgical operation. Some men experience HEMATOMA (collection of BLOOD within the scrotum) and GRANULOMA (SCAR tissue formation) after vasectomy. Most hematomas reabsorb within a week. Granulomas develop in reaction to sperm that leak into the tissues within the scrotum from the cut end of the vas deferens. Though granulomas are not harmful, they may remain tender or even painful for several weeks to several months.
Sperm may remain in the seminal ducts and other structures for quite some time, so a vasectomy is not effective immediately. A man must have two negative sperm counts one to two months after the vasectomy (or after 10 to 20 ejaculations) before he can consider himself infertile. It is essential to use an alternative method of CONTRACEPTION during this time. Because reanastomosis (also called recanalization) may occur years to decades after vasectomy, a man who has had a vasectomy should have periodic sperm counts throughout life to confirm that he remains infertile.
Vasectomy Outlook and Lifestyle Modifications
Vasectomy renders a man permanently infertile (sterile) by blocking the route by which sperm travel out of the testicles. Spermatogenesis (production of new sperm cells) continues; the body eventually reabsorbs the sperm. Vasectomy does not alter a man’s sexual desire or erectile function (ability to have an ERECTION). The ejaculate contains about the same amount of SEMEN as before vasectomy; the semen does not contain sperm, which slightly reduces its volume. There is a very slight risk for spontaneous reanastomosis (reconnection of the cut ends of the vas deferens) that can result in unexpected FERTILITY. Surgery to reverse vasectomy is sometimes possible to restore fertility, though multiple variables affect its success. Men should consider the loss of fertility with vasectomy to be permanent. Vasectomy does not provide protection against infection with SEXUALLY TRANSMITTED DISEASES (STDS) or HIV/AIDS.
See also FAMILY PLANNING; SEXUALLY TRANSMITTED DISEASE (STD) PREVENTION; SURGERY BENEFIT AND RISK ASSESSMENT; TUBAL LIGATION.