Testicular cancer - symptoms and treatment
What is Testicular cancer
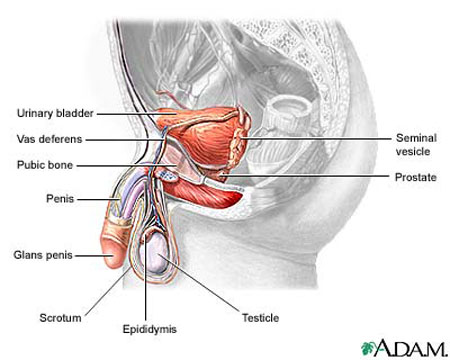
Testicular cancer - A malignant (cancerous) tumor that arises from the tissue of a man’s testicle. Testicular cancer is usually unilateral (occurs only in one testicle), though sometimes occurs bilaterally (in both TESTICLES), and is most common in early adulthood (ages 20 to 34). With detection before the cancer metastasizes (spreads elsewhere in the body), the cure rate for testicular cancer is 99 percent. Doctors in the United States diagnose testicular cancer in about 8,000 men each year.
The two main types of testicular cancer are seminoma and nonseminoma, though some testicular cancers contain a mix of these types. Oncologists classify mixed testicular cancer tumors as nonseminoma because the nonseminoma cells tend to be dominant in determining the tumor’s behavior. The distinction is important because the types have different patterns of aggressiveness (rate and way in which the tumor grows), METASTASIS, and responsiveness to treatment.
Symptoms of Testicular cancer and Diagnostic Path
The most common symptom of testicular cancer is a painless though sometimes tender lump or swelling in the SCROTUM. The man may discover the lump or swelling during TESTICULAR SELF-EXAMINATION (TSE) or coincidentally, or the doctor may find it during ROUTINE MEDICAL EXAMINATION. Testicular cancer also may cause few symptoms until it has grown and spread outside the testicle, such as to organs in the abdomen. In such circumstances, symptoms may be more generalized and include low pelvic or low back heaviness or pressure, fatigue, and overall sense of not feeling well (malaise).
The diagnostic path typically includes BLOOD tests to look for TUMOR MARKERS (proteins in the blood circulation that suggest the presence of cancer), such as ALPHA FETOPROTEIN (AFP) and lactate dehydrogenase (LDH), and ULTRASOUND of the scrotum, which may indicate whether the growth is fluid-filled (more likely a cyst or HYDROCELE) or solid (more likely a tumor).
Though biopsy (removal of a sample of the tumor’s tissue for laboratory examination) is the means of establishing a cancer diagnosis in most other types of cancer, the risk that the biopsy will cause the release of cancer cells into the blood or LYMPH circulation is very high with testicular cancer because of the circulatory and lymphatic structures of the testicle. The urologist may consider biopsy when both testicles are involved or when a man has only one testicle. In such a circumstance the OPERATION begins as would an inguinal orchiectomy but the surgeon sends a tissue sample for the pathologist to examine and waits for the report of cancer or not cancer before proceeding. Otherwise laboratory analysis of the tumor occurs after removal of the testicle and its spermatic cord. The pathologist then identifies the type and stage of the cancer, which determines appropriate treatment options.
| BASIC STAGING OF TESTICULAR CANCER | ||
|---|---|---|
| Stage | Meaning | Treatment Options |
| stage 0/carcinoma in situ | cancer remains contained in the cells of their origin | radical inguinal ORCHIECTOMY |
| stage 1 | cancer remains confined to a local tumor in one testicle | radical inguinal orchiectomy seminoma: inguinal and retroperitoneal LYMPH NODE irradiation nonseminoma: retroperitoneal lymph node dissection or two cycles of chemotherapy |
| stage 2 nonbulky | cancer has spread to retroperitoneal LYMPH nodes and nodes are 2 inches or smaller | radical inguinal orchiectomy seminoma: inguinal and retroperitoneal lymph node irradiation nonseminoma: retroperitoneal lymph node dissection, then two cycles of chemotherapy |
| stage 2 bulky | cancer has spread to retroperitoneal lymph nodes and nodes are larger than 2 inches | radical inguinal orchiectomy seminoma: three cycles of chemotherapy nonseminoma: three or four cycles of chemotherapy |
| stage 3 nonbulky | cancer has spread to lymph nodes outside the abdomen and to the LUNGS though all metastasized tumors are 3⁄4 inch or smaller | radical inguinal orchiectomy seminoma: three or four cycles of chemotherapy; RADIATION THERAPY for BRAIN METASTASIS nonseminoma: three or four cycles of chemotherapy; surgery to remove any remaining metastatic tumors |
| stage 3 bulky | cancer has spread to lymph nodes outside the abdomen and nonlung sites such as the LIVER or brain, and some metastasized tumors are larger than 3⁄4 inch | radical inguinal orchiectomy seminoma: four cycles of chemotherapy; radiation therapy for brain metastasis nonseminoma: four cycles of chemotherapy; surgery to remove any remaining metastatic tumors clinical trials |
| stage 4/recurrent | cancer has returned after treatment | surgery for small, isolated metastases high-DOSE chemotherapy |
Testicular cancer Treatment Options and Outlook
Surgery to remove the testicle containing the cancer is the first line of treatment. The operation of choice is radical inguinal ORCHIECTOMY, performed with the man under general ANESTHESIA. The surgeon makes an incision in the groin and pulls the testicle up from the scrotum to remove it, intact, along with its spermatic cord. The spermatic cord contains the blood and lymph vessels that supply the testicle; removing the entire testicular structure significantly reduces the risk for stray cancer cells entering the blood and lymph circulations to spread elsewhere in the body.
For seminomas or large tumors, the surgeon may also remove lymph nodes in the lower abdomen that are the path of lymph drainage from the spermatic cord (retroperitoneal LYMPH NODE dissection). Though a more extensive surgery, such an operation is very successful in preventing the spread of the cancer.
Most men then receive adjuvant (accompanying) treatment with RADIATION THERAPY or CHEMOTHERAPY, depending on the type and stage of the cancer. Tumors that contain only seminoma cells (pure seminoma) tend to stay contained longer and are very sensitive to radiation therapy. Tumors that contain nonseminoma cells tend to metastasize (spread) earlier and are more responsive to chemotherapy. Oncologists typically administer chemotherapy using combinations of drugs for several cycles (three or four) of treatment.
| CHEMOTHERAPY AGENTS TO TREAT TESTICULAR CANCER | |
|---|---|
| bleomycin | carboplatin |
| cisplatin | cyclophosphamide |
| etoposide | ifosfamide |
| vinblastine | |
Testicular cancer is among the most treatable cancers. Testicular cancer detected and treated while it remains localized in one testicle (stage 0 or stage 1) has a current five-year survival rate of 99 percent; oncologists consider this a cure rate because the cancer rarely recurs. The RECURRENCE rate (likelihood for the cancer to return after treatment) is very low, though a man who has had testicular cancer has increased risk for cancer in the remaining testicle (usually a new cancer rather than a metastasis of the original cancer) or for other types of cancer.
Treatment for testicular cancer does not affect a man’s sexuality though may affect his FERTILITY. Most people feel fatigued during cancer treatment, which often lowers LIBIDO (interest in sexual activity). However, most testicular cancer treatments do not affect a man’s ability to obtain ERECTION, reach orgasm, or achieve EJACULATION. Extensive retroperitoneal lymph node dissection has a slight risk for NERVE damage that can result in RETROGRADE EJACULATION (in which SEMEN enters the BLADDER rather than exiting the PENIS during ejaculation). Many men retain fertility after testicular cancer, though doctors recommend sperm banking for men who may desire to father children because many factors influence fertility so it is not certain. A man may choose to have a testicular prosthesis implanted to restore the cosmetic appearance and feel of the scrotum.
Risk Factors and Preventive Measures
The most significant risk factor for testicular cancer is undescended testicle (CRYPTORCHIDISM), even after corrective treatment. Untreated cryptorchidism in which the testicle remains within the abdomen presents a very high risk as well as low potential for early detection of testicular cancer. Testicular atrophy, such as may occur after INFECTION with the MUMPS VIRUS, bacterial ORCHITIS, or SEXUALLY TRANSMITTED DISEASES (STDS), and family or personal history of testicular cancer also increase a man’s risk for testicular cancer. Though there are no measures to prevent testicular cancer, monthly TSE is an effective means of early detection. Regular follow-up care, including blood tests to measure tumor markers and imaging procedures such as COMPUTED TOMOGRAPHY (CT) SCAN or POSITRON EMISSION TOMOGRAPHY (PET) SCAN, is important.
See also BREAST CANCER; CANCER TREATMENT OPTIONS AND DECISIONS; HORMONE-DRIVEN CANCERS; PROSTATE CANCER; SEXUAL HEALTH; STAGING AND GRADING OF CANCER; SURGERY FOR CANCER.